REPLY to Question: How to lower anti-spike IgG antibodies which appear to correlate with adverse effects
We should all try to avoid "Hypersensitivity Myocarditis after COVID-19 mRNA Vaccination" J Clin Med. 2022 Mar PMCID: PMC8949349 DOI: 10.3390/jcm11061660
I intend to reply to all questions offered at the “ask me anything” post; let’s use that post as the central hub for questions and I will get to them as soon as I can:
Here, you’ll find the original post, followed by my reply and any supporting info.
Original question:
My question is this: are you aware of any interventions that can bring down the # of circulating spike IgG antibodies? It appears to me that the higher the number of circulating AB, the more severe the pathology is in my patients. The current highest with 25,000+ has advanced metastatic soft tissue sarcoma that recurred ––from an initial resolved state in 2002––after her booster within 2 months. The "howbadismybatch" website matched, as both of her early injections were identified as batches with very high adverse events.
Finally, have you seen any data that correlates the amount of spike protein with the # of antibodies?
No rush to answer, enjoy your family and friends and wishing you a wonderful celebration!
Reply:
Thank you, by all accounts, I appear to have survived my first and hopefully my only wedding. The bride was charming as always, and I actually got a little bit emotional but pulled myself together.
I appreciate your question and I would like to think or at least hope that by now everyone in the medical world is aware of the relationship between these experimental injections and their inherent toxicity because they are designed to actually produce a toxic protein that triggers inflammation at least and autoimmunity at worst. Actually I guess other things could be worse, like sudden death.
1. Plasma exchange or plasmapheresis
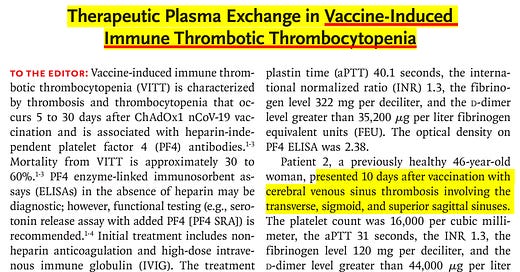
Depending on the urgency of the situation and its severity, the most rapid way to reduce the antibody levels would be plasma exchange or plasmapheresis. In fact, you can see citation to the use of plasma exchange against Cv19-Vaccine-Induced Immune Thrombotic Thrombocytopenia (Cv19-VITT) in the August 26, 2021 excretion of New England Journal of Medicine which I have linked here nejm.org/doi/full/10.1056/NEJMc2109465
Relatedly, we can also note: Plasmapheresis reduces cytokine and immune cell levels in COVID-19 patients with acute respiratory distress syndrome (ARDS) Pulmonology. 2021 Nov-Dec;27(6):486-492 doi: 10.1016/j.pulmoe.2020.10.017
2. Steroids, prednisone and its derrivatives
Anti-inflammatory steroids are commonly used against antibody-mediated diseases. Basically they have an anti-inflammatory effect by global inhibition of protein synthesis, and that includes antibodies.
“These findings demonstrate myocarditis hypersensitivity to some component of the vaccine (spike protein?) acting as a hapten to some macromolecules of cardiomyocytes.”
Citation: "Conclusions: Eosinophilic myocarditis is a possible adverse reaction to the mRNA COVID-19 vaccine. Its pathway is mediated by release of cationic protein and responds to short courses of steroid administration." Hypersensitivity Myocarditis after COVID-19 mRNA Vaccination. J Clin Med. 2022 Mar 16;11(6):1660. doi: 10.3390/jcm11061660 PMCID: PMC8949349 DOI: 10.3390/jcm11061660
3. Antiinflammatory Immunomodulation, ie, Chapter 4, the FINDSEX protocol, including fasting
You may have noticed a correlation between vitamin D deficiency and more severe adverse reactions to iatrogenic injections, and the area where this is most clear is in the setting of autism which just so happens to be coincidental after routine injections comprised of antigens, chemicals and highly allergenic drugs, ie the perfect inflammatory cocktail.
In the allopathic medical world, they commonly think that a “higher antibody response” is somehow “better” but I actually interpret this as a manifestation of pre-existing immune dysregulation which of course can be caused by many factors but clearly vitamin D is one of the top five factors involved here.
As such, I suspect that supplementation with several of these protocol components especially vitamin D, vitamin A, lipoic acid and a few others would be of benefit, and you can see the early outline of the protocol in the following video:
4. Colonics? Probably not, but who doesn’t need and love a good colonic?
As I have detailed previously, colonics appear beneficial for stimulating bile flow and that may help with the excretion of IGA antibodies, but that data would not necessarily be applicable against diseases mediated by IgG antibodies.