UPDATE February-March 2025: I’ve noticed that some of the videos previously posted/streaming from the Vimeo platform are no longer reliably visible, while at the same time, this Substack platform has progressively allowed for direct uploading/embedding of videos; as such, many of the previously-posted videos are being reloaded directly into the Substack platform for more reliable access and archiving.
Video #7: Dysbiosis by Location—Genitourinary Tract
Objectives and Clinical Importance:
Be able to define and explain the clinical significance of: Dysbiosis, eubiosis, and the associated terminology in immunology, microbiology, and pathophysiology
Explain: The role of multifocal polydysbiosis in metabolic and inflammatory diseases
Analyze/Interpret: Laboratory results for significance and/or lack thereof; judicious analysis
Identify: Actionable alterations in microbial patterns, phenotypes of dysbiosis-induced disease
Demonstrate: Familiarity with the published research, especially the work of Noah and colleagues as well as Rashid and Ebringer
Implement: Treatment plans consistent with the 4 main components of evidence-based medicine
Clinical narrative: The genitourinary tract is known to be a common location of infection-induced systemic inflammation as appreciated with classic Reiter’s syndrome, which is now termed reactive arthritis. Likewise, available evidence points to the genitourinary tract as a source of microbe-induced immunostimulation in persistent arthritis, such as rheumatoid arthritis.
When I first studied (and later taught) Clinical Laboratory Medicine1 at the graduate/doctorate level, I remember our professor telling us that urine is an excellent culture media for bacterial growth. Stated slightly differently: Urine is a broth of nutrients and hormones, making excellent fertilizer for a wide range of bacteria and fungi. Overgrowth of microbes in the genitourinary tract can trigger/cocreate systemic inflammation and autoimmune diseases. We have classic examples of this.
Reactive arthritis is a general term that describes any chronic inflammatory multi-joint disease (polyarthritis) that is attributable to an infection or microbial colonization at a different location. Obviously, this is not the same as joint infection (septic arthritis) which typically affects only one joint (not several joints) and is typically acute (intense and short-term, not chronic).
The classic prototype of Reactive Arthritis was previously termed Reiter's Syndrome, which describes polyarthritis (inflammation of many joints), oligoarthritis (inflammation of a few joints), spondylitis (inflammation of the spine) or sacroiliitis (inflammation of the pelvis), in response to a genitourinary infection, typically chlamydia. The infection does not have to be localized to the genitourinary tract, although Reiter syndrome implies this; the infection or colonzation can occur in the gastrointestinal tract for example with Giardia parasite colonization or Salmonella or Shigella infection.
No-one in medicine denies the existence of reactive arthritis; it is considered rare, but is obviously very real. But it is not really obvious. Most clinicians can make the diagnosis of reactive arthritis if they are presented with the classic presentation of a young man/woman presenting with the combination of a new sexually transmitted infection plus joint pain, especially in the low-back, pelvis, hips, knees and/or ankles. You’d expect that type of case presentation on medical licensing exams.
“Reactive arthritis, also called Reiter's syndrome, is the most common type of inflammatory polyarthritis in young men. It is sometimes the first manifestation of human immunodeficiency virus infection. An HLA-B27 genotype is a predisposing factor in over two thirds of patients with reactive arthritis. The syndrome most frequently follows genitourinary infection with Chlamydia trachomatis, but other organisms have also been implicated. Treatment with doxycycline or its analogs sometimes shortens the course or aborts the onset of the arthritis. Reactive arthritis may also follow enteric [gastrointestinal] infections with some strains of Salmonella or Shigella, but use of antibiotics in these patients has not been shown to be effective. Reactive arthritis should always be considered in young men who present with polyarthritis.” American Family Physician 1999
The question/issue becomes who among which doctors can diagnose a nonclassic clinical presentation, a more complex case, perhaps complicating the appreciation of the relationship by labeling the patient with some official (yet largely meaningless) diagnostic tag such as:
Rheumatoid arthritis (RA)
Psoriasis, psoriatic arthritis (PsA)
Ankylosing spondylitis (AS), spondylitis
All videos are being re-uploaded in Feb-Mar 2025 to provide direct and reliable access through the substack platform:
Microbiome Dysbiosis (1) Course Overview and Introduction to Major Concepts and Mechanisms
Microbiome Dysbiosis (3) Prototypes of Dysbiosis-Induced Disease (VIDEO:1hour,42minutes=102minutes)
this current page
My course on “Human Microbiome and Dysbiosis in Clinical Disease” was developed over several years starting formally in 2015-2017 as a continuing medical education (CME) postgraduate online conference joint-accredited for doctors, nurses, and pharmacists:
“American Medical Association Physician's Recognition Award (AMA PRA) Category 1 Statement: This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership … accredited by the ACCME to provide continuing medical education for physicians. …designates this educational activity for a maximum of 30 AMA PRA Category 1 credits.
Nursing Statement: …approved provider of continuing nursing education by the Washington State Nurses Association WSNA A-CNE, an accredited Approver of Continuing Nursing Education.
Pharmacy Statement: …accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. Objectives appropriate for pharmacists.”
I’ve established legitimate expertise on this topic for more than 20 years via clinical experience, post-graduate conference presentations, book publications, and numerous peer-reviewed professional publications.
Dr Alex Vasquez. Reducing pain and inflammation naturally - Part 6: Nutritional and Botanical Treatments Against “Silent Infections” and Gastrointestinal Dysbiosis, Commonly Overlooked Causes of Neuromusculoskeletal Inflammation and Chronic Health Problems. Nutritional Perspectives 2006 Jan
Dr Alex Vasquez. Neuroinflammation in fibromyalgia and CRPS is multifactorial. Nat Rev Rheumatol 2016 Apr;12(4):242. doi: 10.1038/nrrheum.2016.25 pubmed.ncbi.nlm.nih.gov/26935282
Dr Alex Vasquez. Biological plausibility of the gut-brain axis in autism. Ann N Y Acad Sci 2017 Nov;1408(1):5-6. doi: 10.1111/nyas.13516 pubmed.ncbi.nlm.nih.gov/29090837
Dr Alex Vasquez. Musculoskeletal Pain: Expanded Clinical Strategies: Printed monograph approved for ACCME PRA-1 Continuing Medical Education ncbi.nlm.nih.gov/nlmcatalog/101633549 Published by: Institute for Functional Medicine. 2008 May
Dr Alex Vasquez. Mitochondrial Medicine Arrives to Prime Time in Clinical Care: Nutritional Biochemistry and Mitochondrial Hyperpermeability ("Leaky Mitochondria") Meet Disease Pathogenesis and Clinical Interventions. Integr Med (Encinitas) 2014 Aug;13(4):44-9 pubmed.ncbi.nlm.nih.gov/26770108
Dr Alex Vasquez. Reply to "role of Western diet in inflammatory autoimmune diseases" by Manzel et al. In current allergy and asthma reports (volume 14, issue 1, January 2014). Curr Allergy Asthma Rep 2014 Aug;14(8):454. doi: 10.1007/s11882-014-0454-4 pubmed.ncbi.nlm.nih.gov/24947682
Dr Alex Vasquez. Correspondence regarding Cutshall, Bergstrom, Kalish's "Evaluation of a functional medicine approach to treating fatigue, stress, and digestive issues in women" in Complement Ther Clin Pract 2016 May. Complement Ther Clin Pract 2018 May;31:332-333. doi: 10.1016/j.ctcp.2016.10.001 pubmed.ncbi.nlm.nih.gov/27814977
Dr Alex Vasquez. The Microbiome Arrives to Prime Time in Primary Care, Implications for the Anti-Dysbiotic Treatment of Fibromyalgia. Nutritional Perspectives 2015 Oct
Dr Alex Vasquez. Translating Microbiome (Microbiota) and Dysbiosis Research into Clinical Practice: The 20-Year Development of a Structured Approach that Gives Actionable Form to Intellectual Concepts. International Journal of Human Nutrition and Functional Medicine 2015 Jun



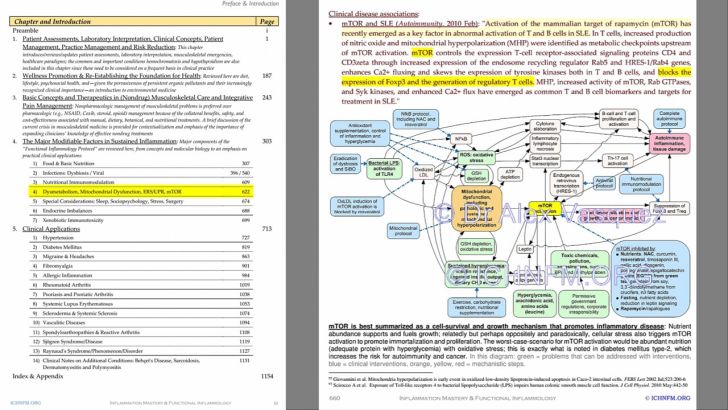
Currently, my largest and most detailed explanation of dysbiosis-microbiome is in Inflammation Mastery 4th Edition currently available at discounted price directly from the publisher:
Sample PDF downloads:
Click here to see the first few pages, including the table of contents and index (size: 6 MB)
Click here for a larger sample with photos (size: 43 MB)
[TUTORIAL VIDEO] Integrating Functional-Naturopathic Medicine into Medical Practice for Specialty and Primary Care [IM4update]
Here is another Update to IM4 = Inflammation Mastery, 4th Edition (available from BookDepository, Amazon, Barnes and Noble, ThriftBooks, AbeBooks, BetterWorldBooks, WaterStonesBooks)
[Adding a paywall line is necessary due to changes in Substack formatting requirements but nothing is added below this line]
nothing is added below this line




![[TUTORIAL VIDEO] Integrating Functional-Naturopathic Medicine into Medical Practice for Specialty and Primary Care [IM4update]](https://substackcdn.com/image/fetch/$s_!v4bh!,w_1300,h_650,c_fill,f_auto,q_auto:good,fl_progressive:steep,g_auto/https%3A%2F%2Fsubstack-video.s3.amazonaws.com%2Fvideo_upload%2Fpost%2F125753986%2Fff68a1b4-4785-47f6-ac2b-deab1cf20c8f%2Ftranscoded-00001.png)








