Quick Consult on IRON DEFICIENCY: Discussion and Diagram
Iron deficiency in adults is commonly the first manifestation of bleeding from an undiscovered gastrointestinal cancer; as such, all iron deficiency requires professional evaluation
Iron deficiency is relatively common worldwide in all age groups and can occur in both genders although it is more common in women, mostly due to blood loss through menstruation and childbirth. Iron deficiency occurs as a result of 1) insufficient intake, including blocked absorption, and/or 2) increased iron loss via blood loss, which is either physiologic or pathologic.
Iron deficiency occurs as a result of 1) insufficient intake, and/or 2) increased iron loss via blood loss, which is either physiologic or pathologic.
Dietary insufficiency of iron is common, especially among persons who do not consume enough meat for economic or personal/ethic reasons. High intake of dietary “fiber” (phytic acid), tea (tannic acid), calcium (supplements) can also reduce iron absorption. More rarely, impaired iron absorption might occur via insufficiency of stomach acid (to support digestion and absorption efficiency) or from intestinal malabsorption due to intestinal disease.
Iron loss through blood loss occurs physiologically (menstruation, childbirth) or pathologically (injury, gastrointestinal bleeding, renal loss). Women experience more iron deficiency because of menstruation, childbirth, and relatively lower consumption of meat whereas men are relatively protected from iron deficiency but tend to suffer more from iron overload (discussed here).
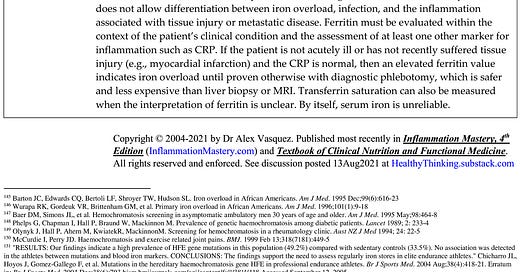
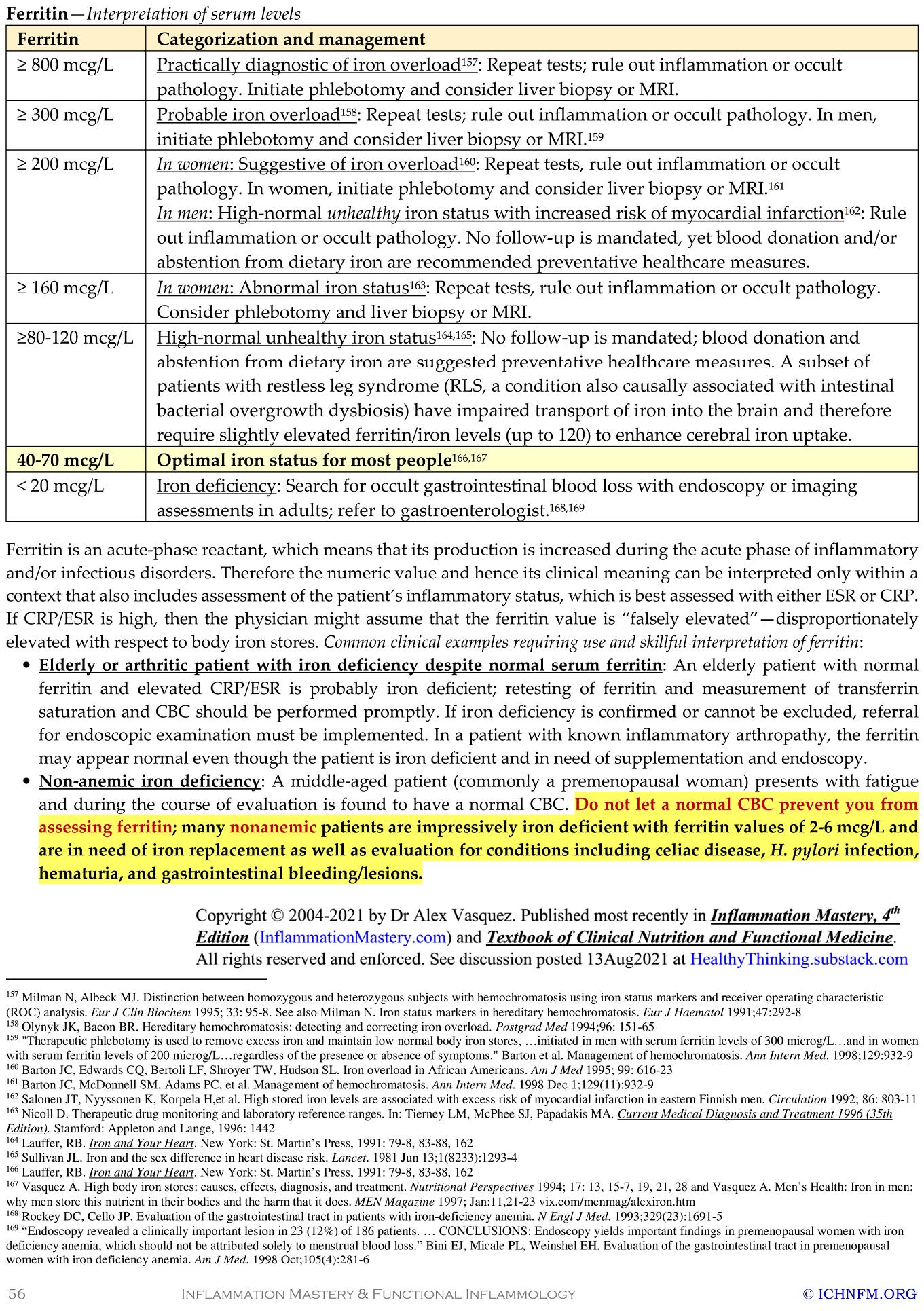
Assessment of iron status is best performed by the laboratory test “serum ferritin”—see interpretive table and diagram below
Assessment of iron status is best performed by the laboratory test “serum ferritin”, which is a common blood test. Other tests such as serum iron and transferrin are not as accurate and more difficult to interpret; serum ferritin is clearly and irrefutably the best blood/laboratory test for iron deficiency (and iron overload—discussed here).
Iron deficiency causes the following problems:
Fatigue: Iron deficiency causes fatigue via any combination of anemia, hypothyroidism (cellular), mitochondrial impairment, and insufficiency of neurotransmitters, especially dopamine.
Depression: Iron is necessary for the formation of dopamine; lack of dopamine promotes a feeling of tiredness, apathy, and depression.
Mitochondrial impairment: Iron is necessary for the proper function of the mitochondrial electron transport chain.
Hypothyroidism (functional): Iron is necessary for the proper function and metabolism of thyroid hormones.
Immune suppression: Iron deficiency causes suppressed immune function and increased risk of infection.
Anemia: Lack of iron typically but not always results in anemia, specifically of the microcytic (small cell) and hypochromic (lack of color) type. However, other diseases can also cause microcytic hypochromic anemia. Impressively, some patients with severe iron deficiency (eg, ferritin of 5, which is extremely deficient) will not have any anemia whatsoever.
Management of iron deficiency always requires two components: 1) determination of the cause, excluding pathologic cause, and 2) iron replacement therapy.
Management of iron deficiency always requires two components: 1) determination of the cause, excluding pathologic cause, and 2) iron replacement therapy. Determining the cause of iron deficiency always requires consideration of pathologic causes, even in children, and especially in menstruating/premenopausal women. As a general rule, all adults with iron deficiency must be considered to have pathologic blood loss (ie, from gastrointestinal bleeding) until proven otherwise; failure to assess for such occult blood loss presents a health risk to the patient and a medicolegal risk to the clinician—this is even more true now that the incidence of colon cancer is increasing among younger people.
As a general rule, all adults with iron deficiency must be considered to have pathologic blood loss (ie, from gastrointestinal bleeding) until proven otherwise
Replacement: Iron replacement is typically achieved with iron supplementation, for example 60 mg 1-3 times per day orally with food (especially meat, to increase absorption); treatment can be pursued every day or every other day. Administration of iron every two days is more efficient than administration daily because less frequent dosing reduces gut accommodation to higher intakes which reduces absorptive efficiency. In very rare situations, patients may need to receive iron by intramuscular injection or intravenous route.
Risks: Iron administration can promote disease among people with bacterial infections or cancer because iron stimulates the growth of some bacteria and cancer cells; in these (somewhat rare) situations, iron administration has to be used judiciously with consideration of timing (eg, preferably after treatment of any infection) and assessment of risk:benefit ratios. Iron supplementation should never be used indiscriminately without supporting evidence of iron deficiency (low levels of serum ferritin) or unless the situation is perfectly clear (exacerbation of anemia following massive blood loss during childbirth). Iron supplementation should be professionally supervised and must always be described in writing with clear instructions to limit supplementation to a specific duration of for example 2-3 months so that patients don’t mistakenly continue taking iron for long periods of time and then suffer iron overload/toxicity. Iron supplements must always be kept out of reach of children; iron toxicity from iron supplements is one of the most common causes of fatal childhood poisonings.
Iron supplementation should be professionally supervised and must always be described in writing with clear instructions to limit supplementation to a specific duration of for example 2-3 months so that patients don’t mistakenly continue taking iron for long periods of time and then suffer iron overload/toxicity. Iron supplements must always be kept out of reach of children; iron toxicity from iron supplements is one of the most common causes of fatal childhood poisonings.


Dr Alex Kennerly Vasquez (introduction; brief Bio-CV) writes and teaches for an international audience on various topics ranging from leadership to nutrition to functional inflammology. Major books include Inflammation Mastery, 4th Edition (full-color printing, 1182 pages, equivalent to 25 typical books [averaging 60,000 words each]), which was also published in two separate volumes as Textbook of Clinical Nutrition and Functional Medicine (Volume 1: Chapters 1-4; Volume 2: Chapter 5—Clinical Protocols for Diabetes, Hypertension, Migraine, Fibromyalgia, Rheumatoid Arthritis, Psoriasis, Vasculitis, Dermatomyositis and most other major inflammatory/autoimmune disorders); several sections have been excerpted including Antiviral Strategies and Immune Nutrition (ISBN 1502894890) (aka, Antiviral Nutrition [available as PDF download] and Brain Inflammation in Chronic Pain, Migraine, and Fibromyalgia. Dr Vasquez’s books are available internationally via bookstores such as BookDepository, Amazon.com, Barnes and Noble, ThriftBooks, AbeBooks, BetterWorldBooks, WaterStonesBooks and his new Telegram channel is https://t.me/DrAlexVasquez.