
3 reasons to donate blood:
1. You can save someone’s life…
…if they’ve lost too much blood in an accident, surgery,
…if they cannot make enough blood due to illness (such as cancer or renal failure) or treatment such as chemotherapy, which commonly causes anemia (insufficiency of oxygen-carrying red blood cells)
Be a good fellow citizen; we all depend on a robust community blood supply because accidents/illnesses can necessitate this for anybody and everybody.
2. You can improve your own health by removing excess iron
Iron Overload (see details here/below) is a common problem and increases the risk for joint/articular diseases, heart disease, liver disease, diabetes, headaches, mental illness and many types of cancer.
You can easily understand that humans are iron-accumulators (major survival advantage in tough conditions) because throughout history we as humans bled on a regular/daily basis, even if just a little via small cuts and scratches. These days, we rarely bleed, therefore rarely lose iron, therefore we (especially men) tend to accumulate iron, which ultimately feeds free-radical production and also feeds diseases such as cancer and infections, since cancer cells and invading bacteria both need iron for their proliferation.
Conversely, the opposite of iron overload (excess) is Iron Deficiency, which is one of the most common nutritional deficiencies worldwide; iron deficiency is one of the only contraindications/prohibitions against blood donation.
You can see my previous post on Iron Overload which I have included/linked below; iron overload was the topic of my first publications starting with “High body iron stores: causes, effects, diagnosis, and treatment” published in Nutritional Perspectives 1994 and “Musculoskeletal disorders and iron overload disease: comment on the American College of Rheumatology guidelines for the initial evaluation of the adult patient with acute musculoskeletal symptoms. [Letter]” published in Arthritis & Rheumatism—Official Journal of the American College of Rheumatology 1996.
3. You can contribute to scientific research
Commonly, you can elect (or not) to have some of the blood sampled within a scientific study, for example one that is looking to estimate the presence or absence of something (like a current or past infection or other problem) in your national or local population. These studies are valuable, and you personally benefit from this research (whether you know it or not) so you might as well do your part and contribute a few drops.
See my original QUICK CONSULT review on iron overload reprinted below:
IRON OVERLOAD was my first self-directed research topic and was the subject of my first publications; my first feature article was published in Nutritional Perspectives in 1994, a few letters in Townsend Letter for Doctors in 1994-1996, and then my first “big league” journal publication in 1996 in Arthritis & Rheumatism, published by the American College of Rheumatology (PMID: 884387, DOI: 10.1002/art.1780391027). I’ve discussed iron overload in all of my major books (Orthopedics 2004, Rheumatology 2006, Pain 2008, …Inflammation Mastery) and you can download the subsection (PDF) from Chapter 1 here from academia.
Iron overload is one of the most common clinical conditions, with roughly 1 per 7 persons with the mild form of the illness and 1 per 200 persons with the severe form of the illness. Clinical manifestations of severe disease include 1) diabetes, 2) heart failure, 3) liver disease, and 4) musculoskeletal pain while presentations of milder disease can include fatigue, depression, hormonal/reproductive/sexual problems, and increased risk and incidence of infections, heart disease, and cancer.
Terms
Iron overload = any condition of excess iron, ranging from mild to severe
Primary disease = inborn, genetic, from within, familial, hereditary disease
Secondary disease = from outside, acquired; having a different cause; if a person has a secondary disease, then the primary cause is something else
Primary iron overload = resulting from a genetic tendency to absorb too much iron from a normal diet; this is one of the most common genetic traits among humans and is termed “genetic hemochromatosis”
Secondary iron overload = resulting from administration or consumption of excess iron
Homozygous = literally “same genes” meaning that a person has inherited the same trait from both parents; a person can be “homozygous normal” meaning that they have two genes for normal health or no disease, or a person can be “homozygous abnormal” meaning that they have two genes for the trait and are more likely to develop clinical disease; homozygous hemochromatosis occurs in roughly 1 per 200 persons (0.5% of the population)
Heterozygous = literally “different genes” meaning that a person has inherited one normal gene and one abnormal/disease gene and will thus develop a milder/intermediate severity of the disease; heterozygous hemochromatosis occurs in roughly 1 per 7 persons (14% of the population)
IRON OVERLOAD describes any condition of excess iron, ranging from mild to severe; the causes are either “primary” as with the genetic disease hemochromatosis (homozygotes: two affected genes in 1 per 200 persons) or “secondary” as with overconsumption of iron-rich foods and supplements. Most affected people (heterozygotes: two affected genes in 1 per 7 persons) have a mild degree of iron overload that results from a combination of genetic tendency (one gene) for iron accumulation in combination with a diet plentiful in iron (eg, meats).
Iron overload is one of the most common clinical conditions, despite the fact that most people (doctors and patients) essentially never think about it and don’t know how to test and manage it; the genetic forms of the illness affect roughly 1 per 7 persons with the mild form of the illness and 1 per 200 persons with the severe form of the illness. Clinical manifestations of severe disease are the classic quadrad/quadriad of 1) diabetes, 2) heart failure, 3) liver disease, and 4) musculoskeletal pain while presentations of milder disease can include fatigue, depression, hormonal/reproductive/sexual problems, and increased risk and incidence of infections, heart disease, and cancer.
Iron overload is one of the most common clinical conditions.
Presentations of milder disease can include fatigue, depression, hormonal/reproductive/sexual problems, and increased risk and incidence of infections, heart disease, and cancer.
Iron overload occurs in men, women, children of all races/nationalities. Iron accumulation takes time, and therefore the condition can occur in children but is more common in adults. Iron overload can occur in infants and neonates but this is a distinct pathologic/genetic condition and is not the same as the typical hemochromatosis.
Laboratory Testing: The shortest and cleanest description you’ll ever read
Serum FERRITIN: Serum ferritin is clearly the best test single test for iron overload, just as it is for iron deficiency. Ferritin levels are a direct reflection of body iron levels
Serum FERRITIN: Serum ferritin is clearly the best test single test for iron overload, just as it is for iron deficiency. Ferritin levels are a direct reflection of body iron levels; my optimal range is 40-70, with up to 120 being permittable for some people with mental depression. Below 20 is iron deficiency; excess is >200 in a woman and >300 in a man. Treatment decisions and monitoring are most commonly based on serum ferritin for all types of iron overload.
Transferrin saturation (from transferrin and serum iron): Transferrin saturation is a mathematical calculation involving serum iron and measurement of the transferrin protein; anything greater than 50% is suspect for iron overload and requires follow-up testing. Transferrin saturation is affected by the pattern of iron metabolism and is thus more sensitive than is ferritin for detecting genetic hemochromatosis; this is advantageous for research studies of prevalence and for detecting the trait in family members (especially kids) of an index/diagnosed case.
Gene testing: Gene testing is best reserved for 1) research, and 2) specialist-supervised testing in family members of an index/diagnosed case. Several different genes exist for promoting iron overload; therefore, a “negative test result” may have simply tested for the wrong gene. Importantly, a “negative test result” does not exclude phenotypic iron overload; a person can have iron overload without having the testable genetic trait. This is why ferritin—which actually measures the amount of iron in the body—will always be the single most important test.
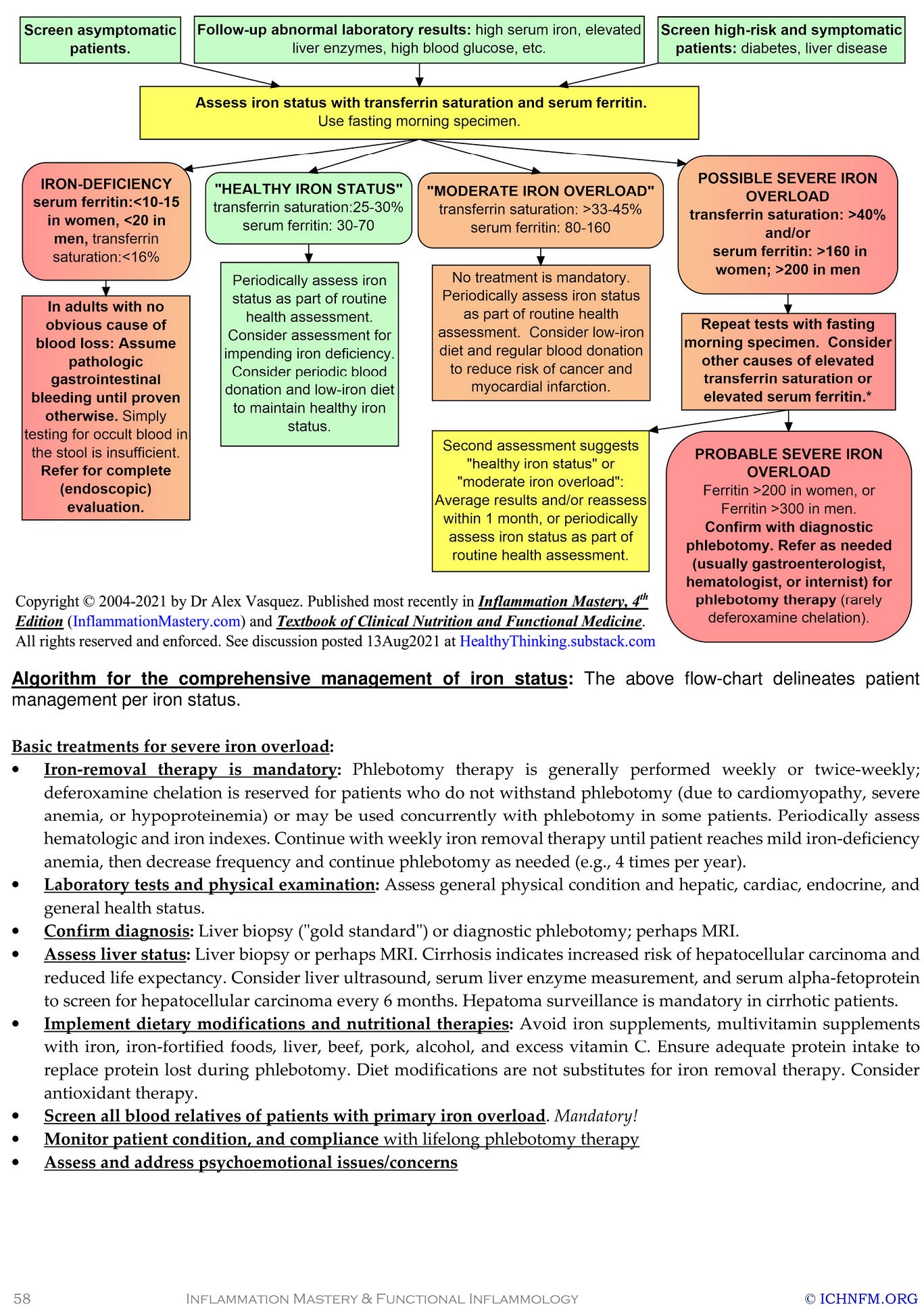
See my laboratory interpretation guide excerpted in the image below, and/or download the subsection from Chapter 1 here from academia.

Dr Alex Kennerly Vasquez (introduction; brief Bio-CV) writes and teaches for an international audience on various topics ranging from leadership to nutrition to functional inflammology. Major books include Inflammation Mastery, 4th Edition (full-color printing, 1182 pages, equivalent to 25 typical books [averaging 60,000 words each]), which was also published in two separate volumes as Textbook of Clinical Nutrition and Functional Medicine (Volume 1: Chapters 1-4; Volume 2: Chapter 5—Clinical Protocols for Diabetes, Hypertension, Migraine, Fibromyalgia, Rheumatoid Arthritis, Psoriasis, Vasculitis, Dermatomyositis and most other major inflammatory/autoimmune disorders); several sections have been excerpted including Antiviral Strategies and Immune Nutrition (ISBN 1502894890) (aka, Antiviral Nutrition [available as PDF download] and Brain Inflammation in Chronic Pain, Migraine, and Fibromyalgia. Dr Vasquez’s books are available internationally via bookstores such as BookDepository, Amazon.com, Barnes and Noble, ThriftBooks, AbeBooks, BetterWorldBooks, WaterStonesBooks and his new Telegram channel is https://t.me/DrAlexVasquez.





