Quick Consult on Acute Vitamin D Optimization: The Goal is Measured in Serum Levels, not Dosage Amounts
The goal of vitamin D3 supplementation is the optimization of vitamin D status and not the administration of any preconceived/fixed amount. Vitamin D status is determined by measurement of serum 25ohD
Executive summary:
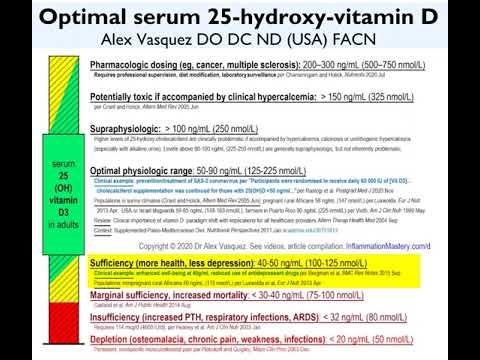
The goal is simple and important: Optimization of serum 25-hydroxyvitaminD levels to at least 50 ng/ml (125 nmol/L) which is protective and physiologic
Method: Administration of vitaminD3 (most common) or 25-hydroxyvitaminD (as available, especially for emergencies); determining dosage for acute infections is determined by situation, availability, and the limited published data reviewed below
Complexity: Described below the images
More details: Articles (academia.edu/40429791) and videos (provided below)
For acute treatment in adults, the available data supports use of either 1) vitaminD3 at 60,000-80,000 IU/d (1,500-2,000 mcg/d) for up to 14 days, or 2) 25ohD at an average of 90 mcg/d for 15 days—see details below


The goal of vitaminD supplementation is the optimization of vitamin D status and not the administration of any preconceived fixed amount.
Adult humans typically metabolize ~4,000 IU per day of vitaminD3 and therefore this amount is a very reasonable “baseline” amount for supplementation. During illness with an infection or any inflammatory disease, vitaminD consumption/metabolism increases as does oxidative destruction of the vitamin, thereby necessitating increased intake. Obesity is another condition that increases the required amount of vitaminD due to a combination of reduced absorption, increased metabolic breakdown, and increased sequestration in adipose tissue. In these situations of increased demand, vitamin D intake commonly has to be increased to 10,000 IU per day as maintenance therapy. One can easily see from these first three examples of infection, inflammation, and obesity that, after respecting a physiologic baseline of 4,000 IU/d, we commonly have to make upward adjustments to the daily vitaminD dose based on increased catabolism, destruction, and distribution, respectively. One would expect to have to increase the orally administered dose for any patient with a malabsorptive condition such as Crohn, celiac, shortened bowel or gut bypass. Thus, daily dosage is a secondary consideration to the primary goal of providing the appropriate amount for the patient’s individualized needs.
Vitamin D status is determined by laboratory measurement of serum 25-hydroxy-vitamin D (25ohD) which is both the storage form of the nutrient as well as being the most biologically active form of the vitamin, in contrast to the most pharmacologically active form of the vitamin which is 1,25-dihydroxy-vitamin D.
More details
Terms:
“Vitamin D” generally refers to Vitamin D3 (cholecalciferol) when discussing oral supplementation and UVB-stimulated dermal production but refers to 25-hydroxyvitamin D when discussing serum levels.
Vitamin D3 (vD3) = cholecalciferol = the form most commonly used in dietary supplements, vD3 is also found in foods such as liver and fish oil; vD3 has very little biological activity prior to being converted to 25ohD in the liver; 1 mcg = 40 IU
25-hydroxyvitaminD3 (25ohD) = calcifediol = calcidiol = also available for oral supplementation in some countries (including by prescription) and also found naturally in some foods; this is the more biologically active form within the human body as it is 3x-5x more potent than vD3 and is the most abundant form of the nutrient in the body; 25ohD is converted to 1,25diohD in the kidney and in other cells, especially activated immune cells; for dosing purposes, conversion of vD3 dosing to 25ohD dosing is complex because these two forms of vitaminD show different pharmacokinetics (eg, absorption, distribution, metabolism, elimination) and different pharmacodynamics (ie, biological potency); as such, for determining clinical use, we have to follow published data, monitor clinical and serum 25ohD responses, tailor the dosing to the situation (eg, acute vs long-term goals) and needs of the patient, especially with regard to absorptive/malabsorptive status, obesity, and infectious/inflammatory status.
1,25-dihydroxyvitaminD3 (1,25diohD) = calcitriol = the most pharmacologically active form of the vitamin, produced in the kidney and distributed systemically in very small amounts while also produced locally in various tissues on an as-needed basis.
For acute treatment in adults, the imperfect data available supports use of either 1) vitaminD3 at 60,000-80,000 IU/d (1,500-2,000 mcg/d) for up to 14 days, or 2) 25ohD at an average of 90 mcg/d for 15 days
For acute therapy—ie, an urgent need to optimize vitamin D status rapidly to confront an acute situation such as a life-threatening viral infection—doses of 60,000 IU per day for 7-14 have been used with good albeit imperfect success (Rastogi et al, Postgrad Med J 2020 Nov), suggesting that a higher dose of 80,000 IU might be more effective. Higher doses of 100,000 IU and above (usually administered once rather than daily) commonly show signals of ineffectiveness or adverse effects, most likely because 1) the system is flooded with the inactive-antagonistic vitaminD3 while simultaneously deficient in 25ohD, and 2) supraphysiologic bolus dosing of D3 activates the 24-hydroxylating enzymes that eliminate/neutralize vitaminD. Direct administration of 25ohD avoids the problem of vitaminD3 antagonism in acute situations and rapidly raises 25ohD levels. Thus, for acute treatment in adults, the imperfect data available supports use of either 1) vitaminD3 at 60,000-80,000 IU/d (1,500-2,000 mcg/d) for up to 14 days, or 2) 25ohD at an average of 90 mcg/d for 15 days per Nogues et al* (J Clin Endocrinology Metab 2021 Jun) who used “Oral calcifediol treatment in soft capsules was administered as follows: first dose of 2 capsules (266 mcg/capsule) at baseline (day 0), a second dose of 1 capsule at day 3, and subsequent doses of 1 capsule given at days 7, 15, and 30” in the acute treatment of Cv19 infection, which was practically identical to the dosing regimen of Castillo et al* in J Steroid Biochem Mol Biol 2020 Oct. *Note that both of these studies—Nogues 2021 and Castillo 2020—were both in the setting of acute Cv19 infection. In the nonacute setting for the treatment of low-back pain, Faraj and Al-Mutairi (Spine 2003 Jan) used 25ohD at 5,000-10,000 IU/d for 90 days with excellent safety and benefits. Valverde et al in J Steroid Biochem Mol Biol 2016 Jan studied four different dosing schedules and showed that 25ohD at 20 mcg/d was the best dose for achieving optimal serum response of 161 nmol/L and 188 nmol/L at 6 and 12 months, respectively, but these patients were not acutely ill (ie, not hyper-metabolizing/catabolizing) nor did they achieve serum 25ohD optimization within a few days as would be necessary for benefit against an acute life-threatening viral infection. Clinicians can use these examples to estimate appropriate treatment while monitoring serum 25ohD levels as appropriate per clinical situation and patient population. As a general rule, when used as a supplement, 25ohD acts faster and is at least 3x-5x more potent (I‘ll use 3.5x) for raising serum 25ohD levels compared with vitaminD3; if we apply this conversion to the daily dose of 25ohD mentioned above in the two Cv19 studies, then 90 mcg x 40 =3600 IU x 3.5 = 12,600 IU of biological vitaminD3 activity, but with immediate activity (no need to wait up to 7 days for conversion of D3 to 25ohD) and no antagonistic effect of the D3 relative to the 25ohD. At 3.5x potency, the 25ohD of 10,000 IU (250 mcg) used by Faraj and Al-Mutairi would have had the biological potency of vD3 of 35,000 IU—a reasonable dose, modestly supraphysiologic, and therapeutically assertive.
The goal of vitaminD supplementation is the optimization of vitamin D status and not the administration of any preconceived fixed amount. The “best approach” therefore starts with determination of acuteness and urgency: if the condition is not acute and life-threatening, then routine vitaminD3 administration (eg, 4,000-10,000 IU/d for adults) is appropriate. If the condition is acute and life-threatening, then the choice is determined by availability of 25ohD, which is faster-acting; dosages of either D3 or 25ohD are initially estimated based on published data (partly and significantly reviewed above) and then tailored to patient need, absorption, size/BMI, and illness with monitoring of clinical signals, serum calcium, and serum 25ohD.
Most of my vitamin D articles are compiled into this single PDF document academia.edu/40429791 while a few others/newer are available from my profile page https://ichnfm.academia.edu/AlexVasquez; note also “Vitamin D3 Pharmacology Infographic” at academia.edu/45175743
For dosing purposes, conversion of vD3 dosing to 25ohD dosing is complex because these two forms of vitaminD show different pharmacokinetics (eg, rates of absorption, distribution, metabolism, elimination) and different pharmacodynamics (eg, biological potency); as such, for determining clinical administration, we have to FOLLOW, MONITOR, and TAILOR:
follow published data, especially the successful clinical trials in Cv19,
monitor clinical and serum 25ohD responses,
tailor the dosing to the situation (eg, acute vs long-term goals), and
tailor the dosing to the metabolic needs of the patient, especially with regard to absorptive/malabsorptive status, obesity, and infectious/inflammatory catabolic status.
Closing Commentary and Prediction
An attentive reader-thinker might have noticed a paradox in the information provided above, namely that the clinical trial published in 2003 using 25ohD against benign low-back pain (n=300) employed a dose of 10,000 IU (250 mcg) yet the two clinical trials published in 2020-2021 against life-threatening Cv19 infection used only 90 mcg. The 2003 study clearly and irrefutably established safety and pharmacologic efficacy among a very large group of patients; so, with safety and efficacy already established, what could possibly be the excuse for using less than half of that established dose for a more severe and urgent condition? I suspect the answer is either benign ignorance, ie, failure to adequately review the background research, or political-financial pressure to use a weak intervention to produce weak results.
Future studies should 1) use higher doses of 25ohD in the treatment of Cv19, 2) use PTH measurement to attempt to predict risk of and response to treatment, and—most obviously—use other nutrients such as zinc 50 mg, selenium 200-800 mcg, vitamin A (as I have described in the Antiviral Nutrition Course), NAC (videos), as well as other macro and micronutrients (eg, diet protocol), including phytochemicals such as those containing licorice, olive extracts, and probably resveratrol/quercetin, already proven to provide safety and benefit.
Dr Alex Kennerly Vasquez (introduction; brief Bio-CV) writes and teaches for an international audience on various topics ranging from leadership to nutrition to functional inflammology. Major books include Inflammation Mastery, 4th Edition (full-color printing, 1182 pages, equivalent to 25 typical books [averaging 60,000 words each]), which was also published in two separate volumes as Textbook of Clinical Nutrition and Functional Medicine (Volume 1: Chapters 1-4; Volume 2: Chapter 5—Clinical Protocols for Diabetes, Hypertension, Migraine, Fibromyalgia, Rheumatoid Arthritis, Psoriasis, Vasculitis, Dermatomyositis and most other major inflammatory/autoimmune disorders); several sections have been excerpted including Antiviral Strategies and Immune Nutrition (ISBN 1502894890) (aka, Antiviral Nutrition [available as PDF download] and Brain Inflammation in Chronic Pain, Migraine, and Fibromyalgia. Dr Vasquez’s books are available internationally via bookstores such as BookDepository, Amazon.com, Barnes and Noble, ThriftBooks, AbeBooks, BetterWorldBooks, WaterStonesBooks and his new Telegram channel is https://t.me/DrAlexVasquez.
Note:
This wonderful information is not personalized health advice and should only be used with professional supervision along with consideration of other information, including my longer discussions of vitamin D use available at academia.edu/40429791 and https://ichnfm.academia.edu/AlexVasquez
I anticipate that updates will be made to this information when new studies are published so please check the corresponding page at HealthyThinking.substack.com periodically for any changes